What is osteoporosis and who is at risk?
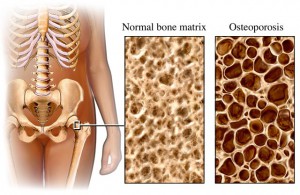 Osteoporosis is a crippling bone disease that results in an increased risk of bone fractures. This is due to a reduction in the density of bone tissue, which is measured as Bone Mineral Density (BMD). Post-menopausal women are at the greatest risk of osteoporosis, due to hormonal changes and age-associated losses of BMD. However, osteoporosis can affect anyone with risk factors including:
Osteoporosis is a crippling bone disease that results in an increased risk of bone fractures. This is due to a reduction in the density of bone tissue, which is measured as Bone Mineral Density (BMD). Post-menopausal women are at the greatest risk of osteoporosis, due to hormonal changes and age-associated losses of BMD. However, osteoporosis can affect anyone with risk factors including:
- Age;
- Gender (post-menopausal women are at the greatest risk);
- How physically active you have been throughout your entire life;
- Eating disorders such as anorexia; and
- Medications that interfere with calcium absorption.
It is alarming to note that in developed countries, the incidence of osteoporosis is increasing faster than the rate at which the population is aging.
How do I reduce my risk?
 A great place to start is by being physically active! Changes in bone mass are directly related to physical activity. Similarly, a sedentary lifestyle is strongly associated with reduced BMD. Physical activity is the only intervention that slows the loss of bone mass and strength, AND reduces the risk of fractures. Prolonged periods of physical inactivity result in decreased BMD as well as gait and balance problems; together, these outcomes increase the risk of falls and increase the risk of subsequent osteoporotic fractures. Recent studies have shown that resistance training programs are also highly effective in improving muscular strength, which helps to decrease osteopenic (lower BMD than normal, but not quite low enough to be considered osteoporosis) and osteoporotic fractures. All of the data points to the importance of physical activity for optimising your bone health, and minimising your risk of osteoporosis.
A great place to start is by being physically active! Changes in bone mass are directly related to physical activity. Similarly, a sedentary lifestyle is strongly associated with reduced BMD. Physical activity is the only intervention that slows the loss of bone mass and strength, AND reduces the risk of fractures. Prolonged periods of physical inactivity result in decreased BMD as well as gait and balance problems; together, these outcomes increase the risk of falls and increase the risk of subsequent osteoporotic fractures. Recent studies have shown that resistance training programs are also highly effective in improving muscular strength, which helps to decrease osteopenic (lower BMD than normal, but not quite low enough to be considered osteoporosis) and osteoporotic fractures. All of the data points to the importance of physical activity for optimising your bone health, and minimising your risk of osteoporosis.
So how much physical activity is needed to reap these benefits for healthy bones? One study has demonstrated that resistance training on 3 non-consecutive days per week for 6 months resulted in increased muscular strength (Bemben et al. 2000). Furthermore, another research group found a significant increase in bone mass and aerobic fitness after one year of training, which consisted of 30 min aerobic activities (e.g., walking, jogging) and 10-15 mins of low intensity strength training (Chow et al. 1987). These results are strongly supported by the American College of Sports Medicine (ASCM), one of the world’s peak sports medicine and sports science organisations. The ACSM recommend exercise throughout all ages, to prevent the occurrence of osteoporosis and aid in the health management of people with osteoporosis.
Balance training is also a critical part of any exercise intervention for bone health, in order to minimise the risk of falls. Improving muscular strength is an effective method for reducing falls and fractures, and for preserving the functional abilities of individuals with osteoporosis. Combining walking with a low intensity resistance training program on 3 days per week can also have a positive impact on your BMD, thereby decreasing fracture risk.
What is resistance training and how do I do it?
 Resistance training involves movements that require a muscular contraction to lift, push, or resist a load. The load can range from medicine balls, to dumbbells, to your own body weight.
Resistance training involves movements that require a muscular contraction to lift, push, or resist a load. The load can range from medicine balls, to dumbbells, to your own body weight.
Following on from the research, it is recommended that resistance training is performed consistently on 2-3 days per week, in order to increase your muscular strength.
At Inspire Fitness, our individually-tailored exercise programs provide you with training to improve your muscular strength while enhancing your balance and stability. Our holistic health approach also addresses postural strength and stability, which combines well with resistance training to ensure your improvement across all aspects related to good bone health.
Author Bio:
Rory Scott is an Accredited Exercise Physiologist at Inspire Fitness for Wellbeing, an Award Winning Gym with Personal Trainers and Exercise Physiologists in Balwyn, Melbourne.
