Written by: Sonja Cornes (Accredited Exercise Physiologist)
In Australia, 1.4 million people are living with diabetes, with approximately 87% of people diagnosed with Type II Diabetes. Developing diabetes is a complex interaction between non-modifiable risk factors such as your genetics, family history, age, and gender, and modifiable risk factors such as your physical activity levels, unhealthy eating patterns, overweight/obesity, smoking and high blood pressure.
What is Type II Diabetes?
Type II Diabetes is a condition characterised by insulin resistance and a gradual reduction of the pancreas to produce insulin. This leads to high levels of sugars (AKA glucose) in the blood. You can think of it as a lock and key system; the pancreas releases the hormone insulin, which is like a key to unlocking a cell to enable the transport of glucose into the cell. When a person develops Type II Diabetes, this key becomes rusted, and it becomes difficult to unlock the cell to allow glucose to enter resulting in those high levels of glucose in the blood.
 The Role of Exercise
The Role of Exercise
There is a plethora of evidence demonstrating the effectiveness of lifestyle changes such as increasing physical activity levels, having a healthy diet, and reducing weight for managing diabetes. The benefits of exercise include:
- Improvement in insulin sensitivity 24-48 hours after exercise
- Increase in muscle mass; an important effect of resistance training, which is increases the muscles storage capacity for glycogen
- Improved body composition by reducing fat mass, particularly visceral fat which will help reduce the risk of developing other chronic diseases
- Increased uptake of glucose into the muscle for energy during exercise
- Improved cardiorespiratory fitness which can reduce cardiovascular risk factors
- Improved mental wellbeing
What are the Recommendations for Exercising with Diabetes?
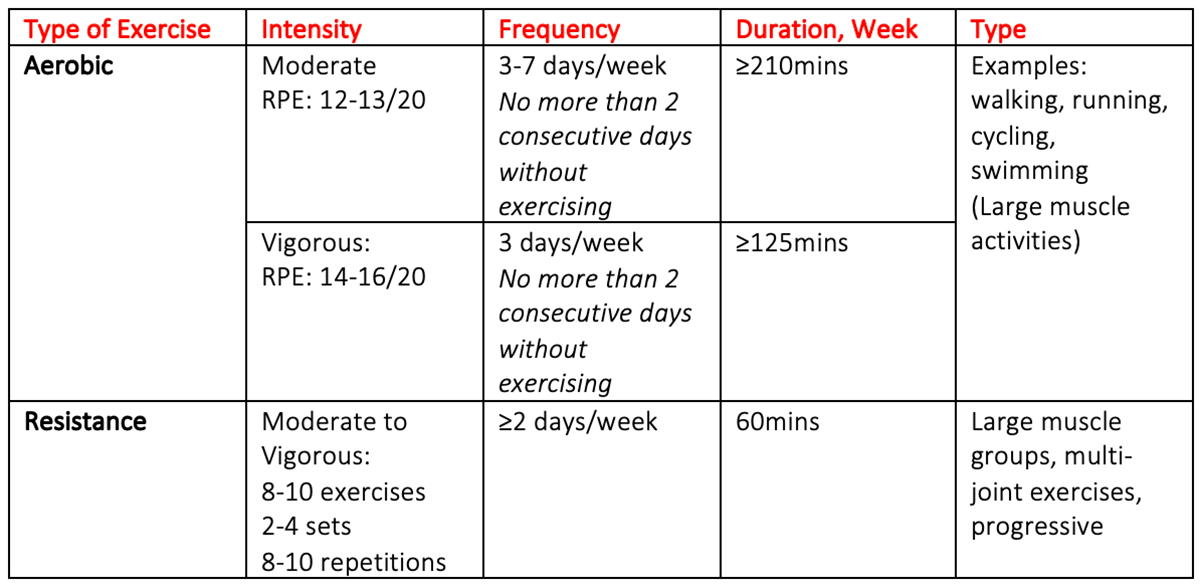
Exercise is safe for persons with diabetes. Evidence suggests that a combination of aerobic and resistance training is important in helping to improve glycaemic control, cardiorespiratory fitness and muscular strength. It is recommended that 150-300mins of moderate to vigorous intensity aerobic and resistance training be completed each week, with no more than two consecutive days without exercising. The exercise recommendations for persons with Type II Diabetes are outlined in the table below (Table 1).
Table 1: ESSA – Exercise and Diabetes (2012)
Special Considerations for Exercise
Exercise plays an integral role in the management of diabetes however, it is important to monitor potential risk factors and co-morbidities when engaging in this activity.
- It is important to monitor your blood glucose levels to ensure it is not too low (AKA hypoglycaemia) or too high (AKA hyperglycaemia). Timing of medication, meals, and exercise sessions can influence these levels. Speak to your doctor and work with your AEP to ensure you can exercise safely.
- Cardiovascular Disease is a common co-morbidity with Type II Diabetes. Prior to undertaking exercise, it essential that an AEP screens for any potential factors that could increase your risk of having a cardiac event during exercise. However, it is important to note risk of having a cardiac event during exercise is relatively small.
How can an Exercise Physiologists help?
Accredited Exercise Physiologists (AEP) form an important part of a multidisciplinary team. They will collaborate with other health professionals such as general practitioners, dieticians, and diabetes educators to provide persons living with diabetes the best possible care and advice to improve their health and wellbeing. AEPs are university trained health professionals who specialise in using exercise to treat, manage and or prevent a number of conditions including diabetes. An AEP will work with you to create an individualised exercise program that reflects your preferences, needs, and goals.
Key Take Aways:
Lifestyle modifications such as improving physical activity levels play a central role in helping to prevent or manage Type II Diabetes. An Accredited Exercise Physiologist can work with you and your health care team to create a treatment plan specific to you. For more information come and have a chat today with one of our AEPs.
Resources for Clients:
Resources for Clinicians:
Bell, K., Shaw, J. E., Maple-Brown, L., Ferris, W., Gray, S., Murfet, G., … & Gordon, B. A. (2020). A position statement on screening and management of prediabetes in adults in primary care in Australia. Diabetes research and clinical practice, 164, 108188.
Hordern, M. D., Dunstan, D. W., Prins, J. B., Baker, M. K., Singh, M. A. F., & Coombes, J. S. (2012). Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. Journal of Science and Medicine in Sport, 15(1), 25-31.
Mendes, R., Sousa, N., Almeida, A., Subtil, P., Guedes-Marques, F., Reis, V. M., & Themudo-Barata, J. L. (2016). Exercise prescription for patients with type 2 diabetes—a synthesis of international recommendations: narrative review. British journal of sports medicine, 50(22), 1379-1381.